Very few treatment modalities have the life-saving prospect of bone marrow transplantation (BMT) in the sphere of medical advances. This procedure has indeed transformed the landscape of treatment for a wide range of serious life-threatening diseases.
Understanding Bone Marrow Transplant
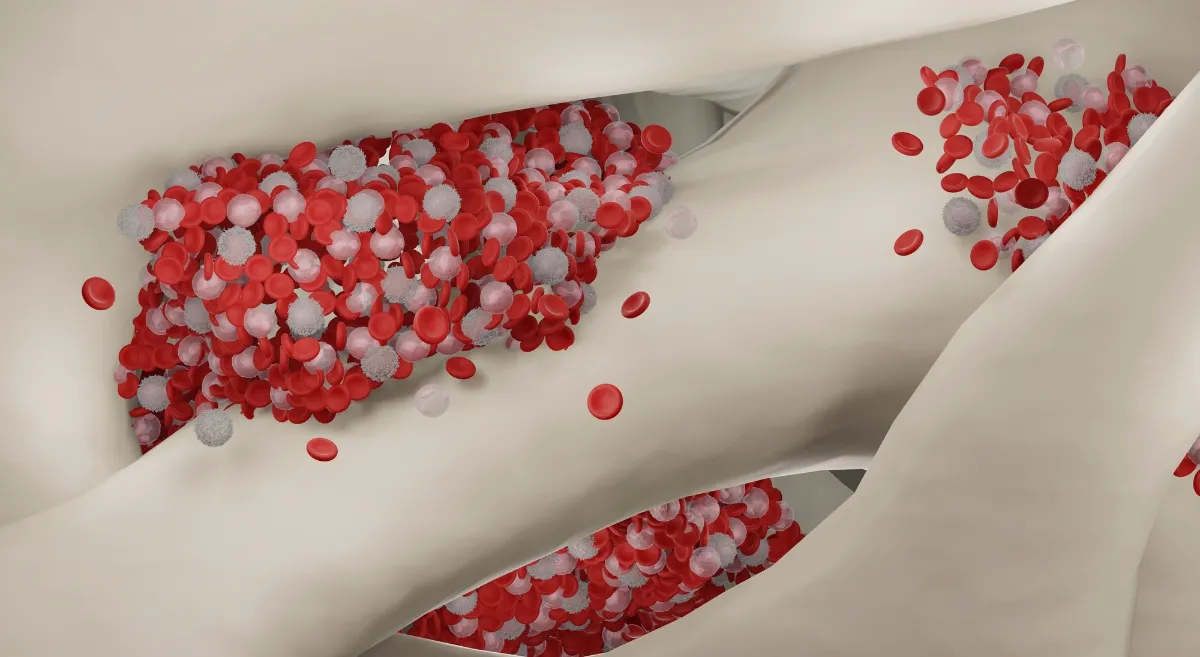
A stem cell transplant, also known as a bone marrow transplant, works by replacing diseased or damaged bone marrow with healthy stem cells. The bone marrow, a spongy tissue located within our bones, is essential to the body's functions, such as blood cell production and immune system regulation. When ailments such as leukaemia, lymphoma, or certain genetic disorders impair its function, a bone marrow transplant can often be curative.
Types of Bone Marrow Transplant
Autologous Bone Marrow Transplant - Autologous transplant uses the patient's own stem cells, which are collected and stored prior to receiving high-dose chemotherapy or radiation treatment. This procedure is especially effective in the treatment of certain cancers such as multiple myeloma and lymphoma. The benefit is an extremely low risk of graft failure and graft-versus-host disease (GVHD), a common complication in other types of transplants. There is also no requirement for an alternate donor.
Allogeneic Bone Marrow Transplant - Allogeneic transplants use stem cells from a compatible donor, who can be related or unrelated. This approach provides a larger pool of donors, increasing the likelihood of finding a good match. Allogeneic transplants have a higher chance of eliminating cancerous cells, but the procedure carries the risk of GVHD. Patient outcomes have improved considerably as GVHD management has advanced.
Haploidentical Bone Marrow Transplant - Haploidentical transplants can be from related or unrelated donors. Half-matched donors, mostly family members, provide stem cells in this novel approach. The treatment has both advantages and disadvantages, including the possibility of a higher risk of GVHD due to the partial genetic match.
Cord Blood Transplant - Cord blood transplants use stem cells extracted from a baby's umbilical cord blood and placental tissue after birth. These cells are frozen and kept for later use. Although cord blood transplants have a lower stem cell count and longer time for engraftment, they provide a greater range of genetic compatibility and are especially useful when a suitable bone marrow donor cannot be found.
Preparing for a Bone Marrow Transplant
A detailed physical evaluation is the first step towards a bone marrow transplant. Medical history, physical examinations, and a battery of tests are used to assess the patient's eligibility and the best transplant type for them. Pre-transplant evaluations ensure that the patient is in good health for the procedure. By eliminating any remaining diseased cells, a conditioning regimen involving high-dose chemotherapy or radiation helps clear the way for new stem cells.
The Bone Marrow Transplant Procedure
The transplant procedure itself is a watershed moment in the patient's journey. Before conditioning therapy, stem cells are extracted from the patient's own blood for autologous transplants. Allogeneic and haploidentical transplants use stem cells derived from the donor's bloodstream or bone marrow. The infusion of healthy stem cells is analogous to a blood transfusion, and it marks the start of a transformative phase. Engraftment, or the process by which transplanted stem cells establish themselves and begin to produce healthy blood cells, is carefully monitored. Complications such as infection, bleeding, or GVHD can occur during and after the transplant. To minimize these dangers, strict medical supervision ensures timely intervention and personalised care.
Recovery and Post-Transplant Care
The time after the transplant necessitates meticulous care and support. Patients are usually hospitalised to closely watch engraftment and manage any complications that may arise. Immunosuppression is used to prevent GVHD while also allowing the transplanted cells to thrive. Supportive care, which includes dealing with side effects and tackling emotional well-being, is critical to the patient's recovery. Once the patient is discharged from the hospital, the focus shifts to long-term follow-up and longevity. Regular check-ups, blood tests, and imaging aid in the success of the transplant and the early detection of any problems. Survivorship includes not only physical recovery but also psychological and emotional healing, enabling the patient to return to normalcy.
Advancements and Future of Bone Marrow Transplant
The field of bone marrow transplantation is constantly evolving, embracing new technologies and techniques. Ongoing research and studies are yielding unique knowledge into personalised treatments, which help to tailor therapies to individual patients based on genetic makeup and disease characteristics. As our understanding grows, the future promises better outcomes and a higher standard of living for transplant recipients.